During my 14 years in the Kentucky House of Representatives, I was deeply involved in overseeing Kentucky’s Medical Assistance Program, better known as Medicaid. I co-chaired a committee that made an in-depth study of Medicaid that resulted in legislation that I sponsored to address waste, fraud, and abuse.
Recently, Medicaid and its recipients have been misrepresented, resulting in divisive and misleading rhetoric. It is crucial that we examine the facts carefully and address the misinformation stemming from recent news reporting and pending legislative actions.
Medicaid funds do not go directly to recipients. Medicaid services prepay for medical care, such as doctor visits, procedures, and medications to aid low-income families, children, parents, caregivers, pregnant women, seniors, and people with disabilities.
The proposal in Congress to cut Medicaid by $625 billion over 10 years, leaving an estimated 7.6 million people without health insurance by 2034, along with the impending work requirements, suggests a lack of sensitivity or understanding regarding the nature of this program and the demographics of Medicaid recipients in Kentucky and nationwide.
History of Medicaid
Let’s begin with a quick overview: Medicaid, established in 1965, is a public insurance program that provides health coverage to low-income families and individuals, including children, parents, pregnant women, seniors, and people with disabilities. It is funded jointly by the federal government and the states. Funds allocated for Medicaid do not go directly to recipients, but are used to pay health care providers on a fee-for-service basis or through prepayment arrangements for medical care.
This includes doctor visits, medical procedures, medications, and more. In Kentucky, the federal government pays about 70% and the state 30% of traditional Medicaid reimbursements, while the match is 90% federal-10% state for expanded Medicaid, allowing Kentucky to provide “significant health care services” at a good value.
The myth of work requirements
Now let’s look at the myth surrounding work requirements for Medicaid care. As the chair of the 1993 Program Review and Investigations Committee and principal sponsor of House Bill 127, an act relating to waste, fraud and abuse, I have consistently kept up with the Kentucky Medicaid Program over the years. It appears a long-standing misconception has produced an effort to create a solution for a problem that does not exist.
Between 2015 and 2017, over 60% of Kentucky Medicaid recipients consistently held full-time or part-time employment. According to 2023 data from the Kaiser Foundation, Kentucky currently ranks 10th in the nation for the number of “working Medicaid recipients.” There are 56.4% with full-time employment and 14.6% with part-time employment. Subsequently, 70.7% of Medicaid recipients are currently working, while 29.3% are not employed.
The non-working group comprises elderly individuals, people with disabilities, children, and caregivers, who together account for approximately 19.8%. These individuals do not meet any of the work requirements currently being proposed. Consequently, the legislative proposals being considered would only affect 9.5% of the remaining Medicaid population here in Kentucky — undoubtedly, a solution for a problem that does not exist.
The real, underlying problem
Work requirements put up barriers to Medicaid coverage. Changes to work and reporting requirements and eligibility criteria have been shown to cause confusion among Medicaid enrollees, leading to substantial coverage loss, even for those who are eligible.
A 2022 Kaiser Family Foundation report revealed that nearly 70% of people who had been dropped from Medicaid lost coverage due to procedural reasons. This is just the latest evidence of the harmful impact on peoples’ access to health care caused by recent changes in Medicaid policy. During the time studied, Kentucky disenrolled 71,000 enrollees for missed paperwork and other procedural reasons. Of these, 74% (52,540) lost coverage attributed to barriers created by the beginnings of a state Medicaid work requirement that a court blocked from taking full effect, while 26% were found ineligible. As a result, 52,540 individuals lost access to health care services.
Clearly, any barriers affecting Kentucky’s Medicaid recipients warrant reevaluation. Our diligent Medicaid recipients merit equitable treatment and consideration.
However, Houston, we do have a problem: Kentucky reported that in 2022, half of working Medicaid enrollees (50%) were employed by companies with over 100 employees and 42.8% worked in the agriculture/service sector. These full-time and part-time workers must rely on Medicaid and SNAP, a nutrition assistance program, because they do not earn a living wage to support their families. Maybe addressing this issue would help find a solution to the real, underlying problem we are currently facing.
The Congressional Budget Office’s analysis shows that the GOP “one big, beautiful bill” will reduce expansion reimbursements, add additional cost to Medicaid recipients, add work requirements, increase coverage barriers, cut Medicaid spending by $625 billion over 10 years, and leave at least 7.6 million more people without health insurance by 2034.
True leadership involves building bridges, not barriers.
--30--
About the author
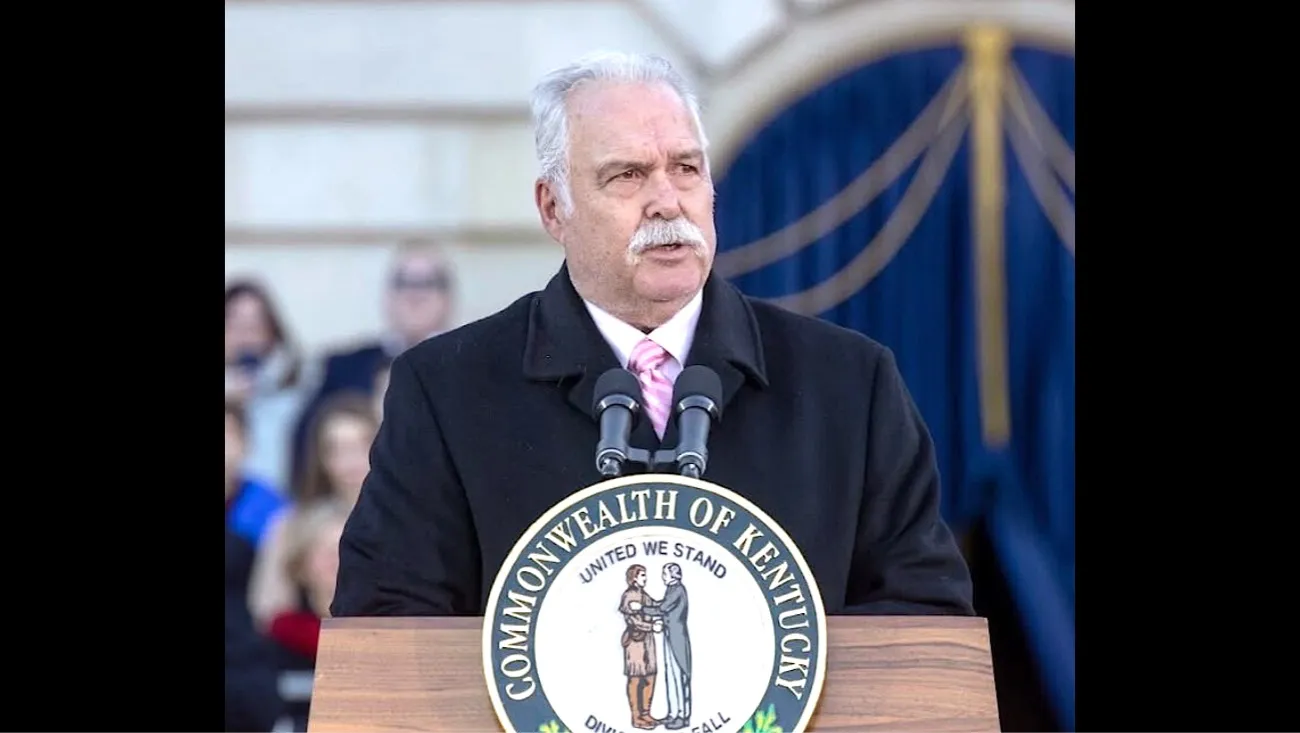
Jack L. Coleman, a Democrat from Harrodsburg, represented Kentucky’s 55th House District from 1991 to 2005. As co-chair of the legislature’s Program Review and Investigations Committee, he helped lead a study of Medicaid that included findings and recommendations concerning financial accountability, recovery and drug utilization. In 1996, he sponsored House Bill 127, an act related to Medicaid waste, fraud and abuse, based on the results of the study. The bill served as a companion to Senate Bill 37, sponsored by then-Sen. Susan Johns, co-chair of the program review committee. Coleman is the father of Lt. Gov. Jacqueline Coleman.
Cross-posted from the Kentucky Lantern.